Glycogenic hepatopathy
A 21-year-old man with type 1 diabetes presented to the hospital with nausea, vomiting, and abdominal pain. Physical exam showed hepatosplenomegaly.
The patient
A 21-year-old man with type 1 diabetes presented to the hospital with nausea, vomiting, and abdominal pain and was admitted for diabetic ketoacidosis (DKA). Vitals on admission were within normal limits; physical exam showed hepatosplenomegaly.
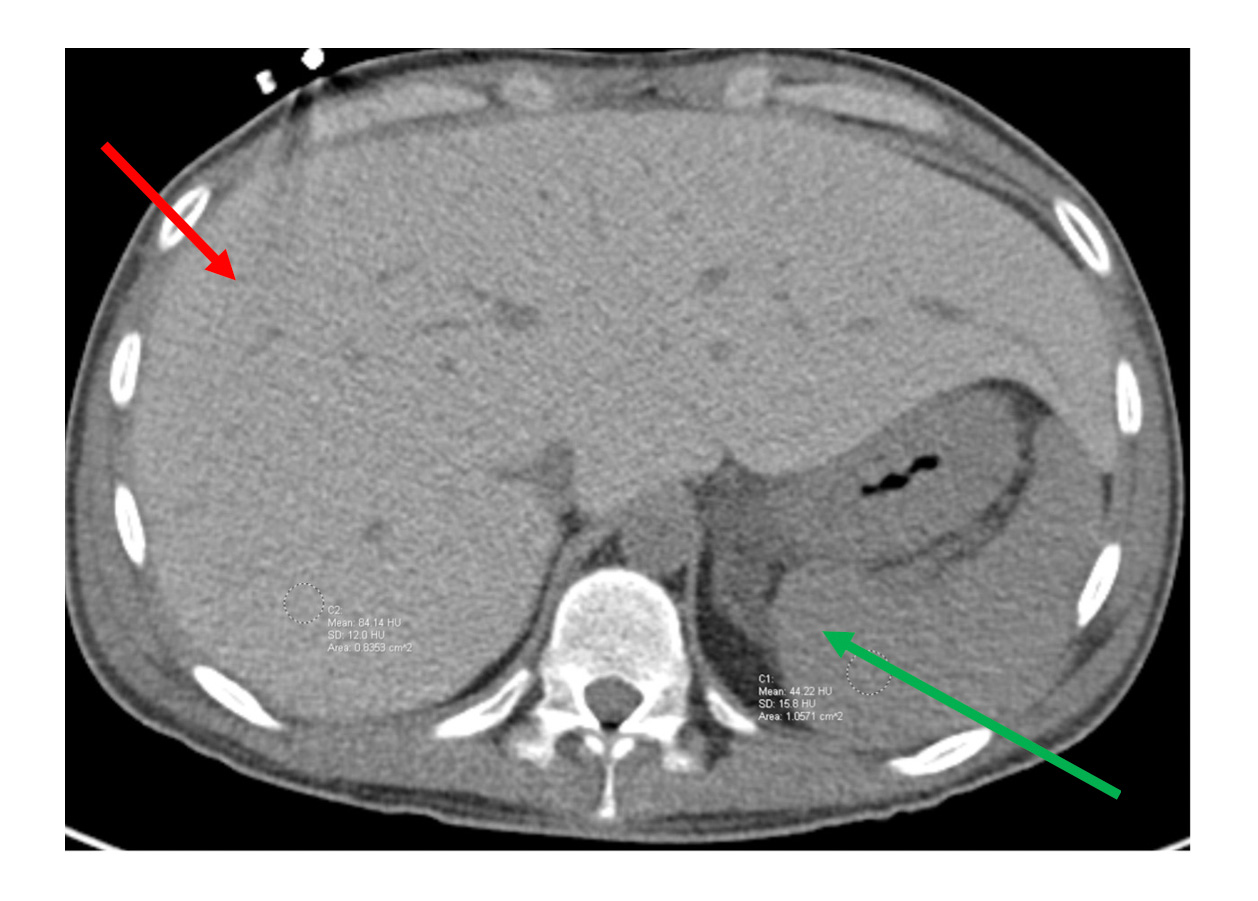
Laboratory studies showed a blood glucose level of 362 mg/dL (reference range, 70 to 120 mg/dL), anion gap of 35 mEq/L (reference range, 5 to 14 mEq/L), pH of 7.02 (reference range, 7.35 to 7.45), aspartate aminotransferase (AST) level of 2,805 U/L (reference range, 0 to 40 U/L), alanine aminotransferase (ALT) level of 678 U/L (reference range, 0 to 41 U/L), HbA1c level of 12.4% (reference range, 4.0% to 6.0%), and lactic acid level of 5.6 mmol/L (reference range, 0.5 to 2.2 mmol/L). Alkaline phosphatase, total bilirubin, albumin, and international normalized ratio were normal. An abdominal CT showed a hyperdense liver (Figure).
The patient was treated with continuous insulin infusion and IV fluid resuscitation. His initial hyperglycemia and ketosis resolved, but his blood glucose remained labile with multiple hyperglycemic and hypoglycemic episodes, as well as persistent lactic acidosis and elevated AST and ALT levels. He later mentioned he had undergone a liver biopsy several months earlier for elevated AST and ALT levels, without follow-up. The pathology report from the liver biopsy was obtained and demonstrated excessive accumulation of glycogen within hepatocytes.
The diagnosis
The diagnosis is glycogenic hepatopathy. This is a rare but underreported complication of poorly controlled diabetes, most commonly type 1. The prevalence of glycogenic hepatopathy is unknown but it is likely underreported because it is conflated with nonalcoholic fatty liver disease (NAFLD). Diabetes is also a strong risk factor for NAFLD, with recent literature estimating its prevalence to be close to 70% in diabetic patients. The majority of case reports of glycogenic hepatopathy are in female patients, and the diagnosis is most often made in young adults.
Glycogenic hepatopathy is most commonly found in diabetic patients and is thought to be related to fluctuations in serum glucose levels, as opposed to simply the presence of hyperglycemia or hyperinsulinemia alone, though the exact pathophysiology of the disease is incompletely understood. Glycogenic hepatopathy can also be a sequela of other metabolic derangements that increase hepatic storage of glycogen, such as dumping syndrome, use of azathioprine or short-term high-dose steroids, anorexia nervosa, or insulin overdose. Excessive levels of glucose and insulin in these disease states activate glycogen synthetase in hepatocytes, which drives excess glycogen synthesis, resulting in hepatomegaly.
Both glycogenic hepatopathy and NAFLD frequently present with hepatomegaly and elevation of aminotransferase levels (AST and ALT) without overt impairment of hepatic synthetic or metabolic function. Glycogenic hepatopathy may be recognized when a patient with DKA presents with aminotransferase levels elevated into the thousands, whereas in patients without DKA aminotransferase levels are only mildly elevated. A focused history with laboratory studies can rule out more common causes of elevated aminotransferase levels, such as a virus or alcohol use, after which NAFLD is often the presumed diagnosis. Other differential diagnoses include hemochromatosis, Wilson's disease, hepatic vein thrombosis, sarcoidosis, and autoimmune hepatitis.
Abdominal CT or MRI can help distinguish glycogenic hepatopathy from NAFLD, as glycogen is a hyperdense substance; imaging in NAFLD will show hepatic hypodensity. Currently, definitive diagnosis of glycogenic hepatopathy requires liver biopsy. Differentiation of the condition from NAFLD is imperative. Glycogenic hepatopathy has an excellent prognosis, with the vast majority of patients' biochemical derangements resolving within days to weeks after improved glycemic control, the mainstay of therapy.
Pearls
- Consider glycogenic hepatopathy in patients with poorly controlled diabetes or recurrent DKA, hepatocellular pattern of liver injury, and a hyperdense liver.
- Recognizing glycogenic hepatopathy is important because it is commonly misdiagnosed as NAFLD but can be reversed with strict glycemic control.
